Next steps for resident doctors in Northern Ireland
In November, the health minister announced that he is now able to proceed with paying this year’s uplift in full for health service staff in Northern Ireland, backdated to 01 April 2025. The award is for a 4% uplift for doctors (plus £750 for resident doctors, which equates to an average 5.4% uplift) and was recommended by DDRB back in May of this year. We have been told this will be in pay packets by February 2026.
While we welcome that the overdue pay uplift for 2025/26 has finally been resolved, it is unacceptable that it has again taken so long to do so. We hope lessons have been learned and the minister’s assurance it will not happen again is not another empty promise.
Although NIRDC (Northern Ireland resident doctors committee) is prioritising contract reform, BMA Northern Ireland will continue to lobby the health minister to ensure your annual uplift is paid on time every year going forward as it is with our colleagues elsewhere in the UK. We will not hesitate to hold the minister to account on this issue and will take whatever action is deemed necessary to ensure that doctors working in Northern Ireland are given their pay uplifts promptly in future and that any uplift continues to make meaningful progress towards Full Pay Restoration.
Our contract, our future
As part of the pay deal for resident doctors that they voted to accept in January 2025, NIRDC and the Department of Health in Northern Ireland (DoH NI) have commenced discussions on negotiating a new contract of employment for residents. Initial planning meetings are currently taking place and once these conclude contract negotiations will commence.
As part of this initial planning stage, NIRDC surveyed all resident doctors in Northern Ireland
to hear what they considered key priority areas for a new contract.
Unsurprisingly, pay and working hours came out as the main priority area residents here want to see improved, followed by better safety limits on working hours, and a more robust monitoring process and better standards of facilities. Access to the timely provision of rotas also featured highly and residents want to see an increase in the allocation and provision of self-development time.
We will continue to update you throughout on these negotiations as they progress.
Read more about contract reform for resident doctors.
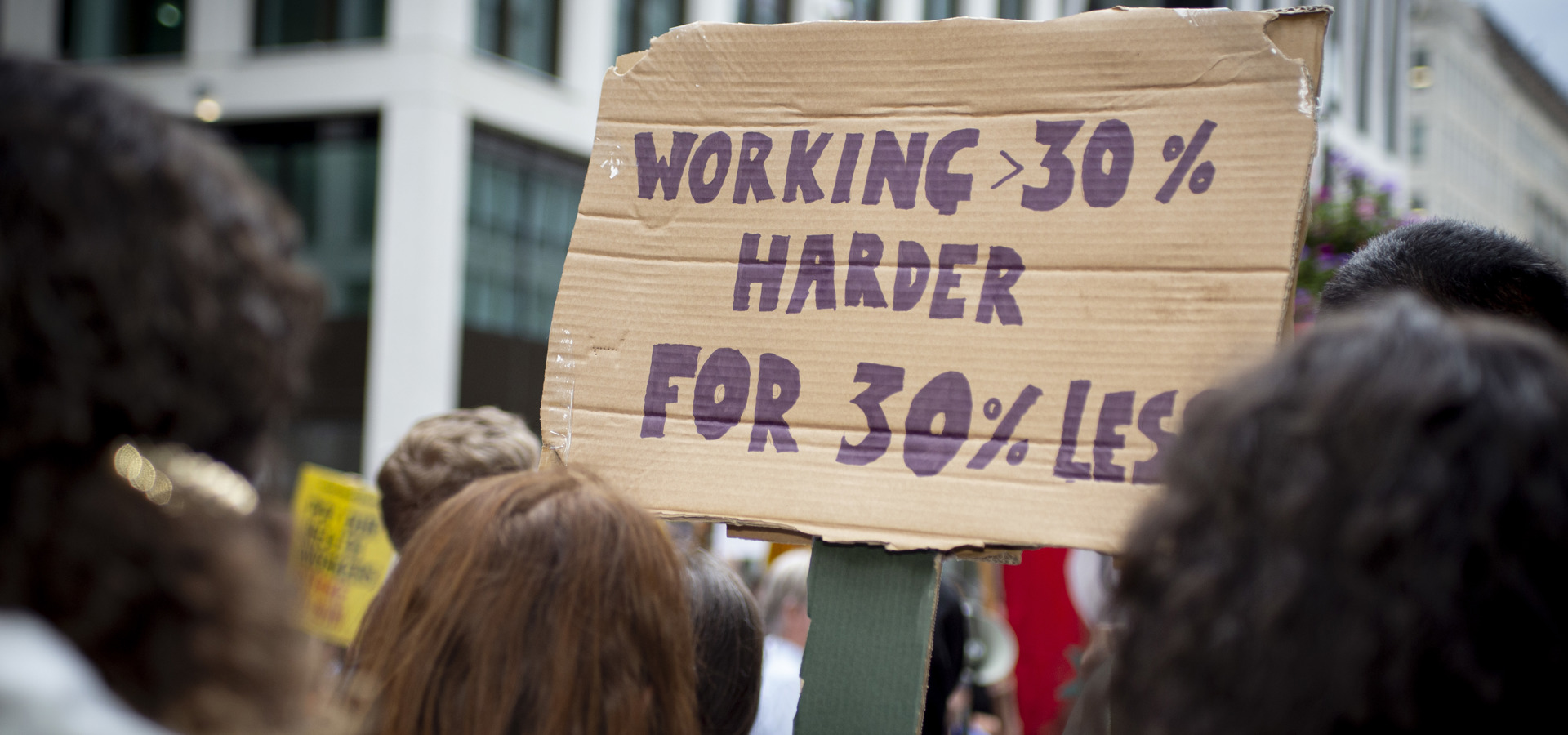
About our campaign
Calculating resident doctor pay erosion in Northern Ireland
Our calculations show that our pay has been eroded by upwards of 20.7% since 2008 when compared with RPI inflation. This is a huge loss to our pay and our living standards that fails to reflect the responsibility, training, and sacrifices required of our work. It’s causing a workforce crisis as fewer and fewer trainees choose to stay in Northern Ireland to train.
The effects of pay erosion
Our pay erosion isn’t just affecting us. It also has an effect on the health service in Northern Ireland. Sub-inflationary pay increases have meant it is now less attractive to work and train in Northern Ireland. We are seeing a workforce crisis emerge from our eroded pay because there are better options elsewhere. This retention and recruitment crisis facing the health service is a risk to its future in Northern Ireland.
2023/24: Delivering change through strike action
In March 2024, for the first time ever, resident doctors in Northern Ireland began the first of three rounds of industrial action to force the DoH NI back to the negotiating table in order to secure a pay deal that would make progress towards pay restoration. After intense negotiations, we were pleased to reach a final deal which 94% of you voted to accept. This deal included an extra 4.05% uplift for all resident doctors pay points, which meant that the 2023/24 pay scales were on average 13.6% higher than in 2022/23. This, alongside the implementation of the 24/25 DDRB recommendation of 6% + £1000 has shown some meaningful progress towards full pay restoration.
We have made some progress to address this erosion, however we continue to call for full pay restoration for resident doctors to at least 2008 levels to make up for this long term, demoralising and undermining deterioration in pay.
Read full details of the accepted negotiated pay deal for 2023/2024.
2024/25: Continuing the path to pay restoration
For the 2024/25 pay year, the DoH NI announced its acceptance of the pay review body’s (DDRB) recommendations on pay. This meant that resident doctors’ pay increased by 6% + £1,000; an in-year uplift of between 7.6% and 9.3% to pay. This pay award was above RPI and therefore continued to restore our pay.
Because of this, and the fact that the uplift continued our path to full pay restoration, we felt that the time was right to bank this pay uplift and further build up our organising capacity. We also began looking at commencing negotiations on an improved contract for resident doctors working in Northern Ireland, which was agreed as part of the pay deal for 23/24.
View the current pay scales, which include the 23/24 additional pay offer and the 24/25 DDRB uplift.
What we're asking for
With better pay, we will incentivise more doctors who studied in Northern Ireland to stay and doctors outside of Northern Ireland to come and work here. With more doctors, our rotas will be less intense, and we will all have more time for training.
We are asking the Department of Health, Employers, and our Assembly to do the following:
This means:
- Full pay restoration for junior doctors in Northern Ireland to 2008 levels.
Read more on pay erosion to see why we're calling for it.
Trusts to commit to complying with the BMA fatigue and facilities charter, with a focus on urgent introduction of safe working limits to fix rotas.
Here's why:
- Junior doctors in Northern Ireland do not have the same rest protections and rota design requirements as elsewhere in the UK. 49% of trainees in Northern Ireland reported working above their rostered hours – higher than the UK average of 42%.
- Exhausting, understaffed rotas impacts on training time required for career development. Significantly more trainees in Northern Ireland (38%) have reported that rota gaps were not being sufficiently dealt with than in the UK as a whole (29%).
Introduction of a trainee guarantee for access to scheduled training, including study leave for F1s.
Here's why:
- Workload pressures are causing the quality of training to deteriorate significantly, particularly for foundation trainees. Almost half (46%) of trainees in Northern Ireland reported significant increase in workload intensity on dayshifts and on nightshifts (20%).
- Lack of training opportunities impacts trainees’ career progression, creating more staffing gaps in higher grades. 21% of trainees in Northern Ireland reported a lack of protected time for completion of all the mandatory training requirements of their post. This was higher than elsewhere in the UK (17%)
- Training protections will be essential to tackling our waiting list crisis.
Commitment from the Department of Health to entering contract negotiations on a reformed junior doctor contract that improves workplace protections, facilities, working hours and recognition.
Here's why:
- The existing contract does not match the reality of training in 2023.
- A new contract is needed that creates a good working environment conducive to training to incentivise junior doctors to stay in training in Northern Ireland.
What you can do
Make sure your details are up to date
It’s vital that we have up-to-date contact details so that we can keep you informed about contract negotiations, ensure you have a vote in any pay or contract referendum, and contact you quickly if a ballot for strike action becomes necessary. Staying connected helps us stay organised and maintain the leverage required to secure a positive outcome.

BMA strike fund - donate now
A strike fund is available to subsidise members in serious financial difficulty who otherwise couldn’t afford to take part in any future rounds of strike action.
The strike fund is supported through voluntary donations to make available to doctors in need.
Keep up to date with our campaign on the NIRDC X (Twitter) and Instagram accounts.

Become a pay activist
-
Help build a team at your workplace that drives our campaign locally.
-
Share your ideas to help BMA Northern Ireland develop our campaign.
-
Recruit new BMA members to strengthen our voice calling for full pay restoration.
-
Join or start local events, meetings and activities in support of the campaign.
Campaign resources
Download a range of campaign materials to share on social media and in your communal work and rest areas.

We're here to stand up for your rights, support you in the workplace and champion the medical profession.