Refugees and asylum seekers can have complex health needs. These may be influenced by experiences prior to leaving their home country, during transit or after arrival in the UK. Holistic and person-centred care is essential to support resilience and help them adapt to life in the UK.
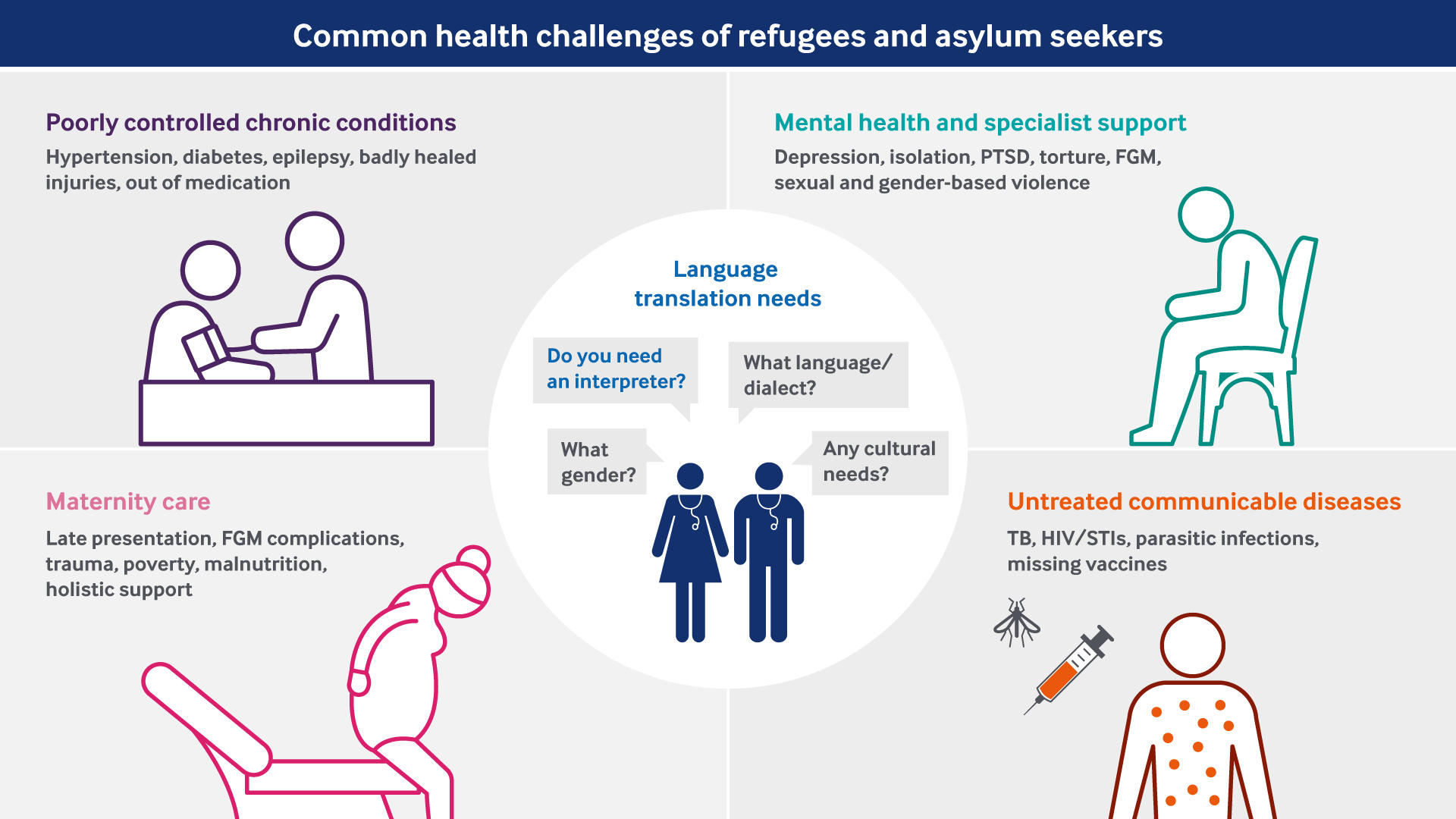
Common health challenges include:
- untreated communicable diseases
- poorly controlled chronic conditions
- maternity care
- mental health and specialist support needs.
Despite this, there is no evidence that refugees and asylum seekers use a disproportionate share of NHS resources, and migrants in the UK and elsewhere in Europe tend to use fewer services than native populations.
If you frequently treat patients who are refugees or asylum seekers, it may be helpful to develop links with specialist patient support organisations locally. See our section on resources for further information.
Communicable diseases
Screening
If you treat refugees and asylum seekers, particularly if you are a GP, it is important to offer screening for infectious diseases that are common in the countries where your patients have spent time before coming to the UK. You may also identify symptoms of communicable diseases when patients present with other routine issues.
In some countries, screening programmes for infectious diseases, such as HIV and hepatitis, may not be easily accessible, or people may not seek testing due to fear of stigma or lack of treatment options.
You should discuss the possibility of receiving a positive result in advance with patients from countries with high rates of certain diseases. PHE’s (Public Health England) Migrant Health Guide includes a section on common communicable diseases and other health issues by country.
Vaccinations
You should also find out what vaccinations refugees and asylum seekers have received. Any missing vaccinations should be offered to children and adults based on the latest UK immunisation schedule.
PHE has developed a practical one-page summary on the best approach to catch-up patients with uncertain or incomplete vaccinations.
Informing patients
As with other patients, you need to inform refugees and asylum seekers about any testing, treatment or vaccinations offered to them.
You may need to take extra care in explaining their rights to confidentiality. For example, you may need to reassure them that a positive result will not negatively affect any asylum application, and that this information is not shared with the Home Office.
Some patients may need additional health education in an appropriate language to understand their options.
You may be able to do this in a consultation using an interpreter, or it may be appropriate to give the patient information leaflets in their language to take away, depending on their literacy level. Specialist patient support organisations may also be able to assist.
Read the section on 'managing language and literacy barriers' for more information.
Resources in other languages
The NHS website provides links to trusted sources of health information in alternative languages. Some NHS Trusts have developed their own range of leaflets in other languages, which may be searchable online.
The Migrant Health Guide also links to leaflets in other languages from specific health topic pages.
Chronic conditions
Refugees and asylum seekers may arrive in the UK with poorly controlled chronic conditions, such as diabetes and hypertension. This is usually the result of long periods without access to regular care, either in their home countries or during their journeys to the UK.
Some patients may have old injuries that have not healed properly. These can cause chronic pain or disability. Untreated dental and eye issues may also cause discomfort or impairment.
Appropriate management
Some conditions may require referrals to secondary care while others will be best managed in primary care.
Many refugees and asylum seekers will be unfamiliar with the way healthcare is organised in the UK. For example, they may expect to be referred to hospital, or be able to self-refer to a specialist, for issues which are normally treated by a GP.
You may need to explain the strength of the UK’s primary care system and the GP’s role in coordinating care.
Maternity care
Pregnancy is often the first significant contact female refugees and asylum seekers have with the UK healthcare system. This is a key opportunity to engage women on a broad range of issues.
Social factors
You should find out about the condition of the patient’s housing and other social determinants of health, especially before discharge following a birth. For example, malnutrition may be a concern due to competing demands for limited funds.
Where health or social welfare concerns are identified, you should consider referring to an appropriate support service.
Female genital mutilation
Additional support may be needed for women who have experienced FGM (female genital mutilation), and their female children if they are considered to be at risk of FGM.
FGM can cause ongoing physical and mental health issues, including complications during pregnancy and childbirth, which should be planned for. It may also deter women from being screened for cervical cancer.
The RCGP (Royal College of General Practitioners) and RCOG (Royal College of Obstetricians and Gynaecologists) both produce guidance for doctors on FGM.
Mental health and specialist support
Most migrants do not experience mental health problems. However, refugees and asylum seekers can be at increased risk, particularly if they have experienced violence and trauma, including exploitation, torture or sexual and gender-based violence.
Issues can range from low to moderate levels of anxiety and depression through to more severe mental disorders. The mental health section of the Migrant Health Guide provides further information and links to resources, including patient information in other languages.
Cultural competence
People from different cultural backgrounds can have different conceptions and experiences of mental illness. For example, patients may complain about non-specific pain or frequent headaches and stomach-aches rather than emotional distress.
In such cases, you should sensitively investigate their history as well as current circumstances to establish whether such complaints may be an expression of mental health or other social issues. This approach can help to minimise unnecessary referrals for investigations and prescribing of medication.
It can be extremely helpful to consider dialect, culture, gender and sexual orientation when selecting a language interpreter. It may also be helpful to link patients with support organisations with expertise in supporting refugees and asylum seekers.
Caring for patients with trauma
Providing care for people who have experienced violence or persecution can be challenging. They may be unable to discuss their health problems openly or be fearful of examination. They may also have difficulty trusting people in positions of authority, including doctors.
Experiences of torture and other violence can cause deep-rooted feelings of shame, humiliation and guilt, and many patients may be reluctant to disclose to a relative stranger. You should respond compassionately and sensitively, and be aware that building a relationship of trust and support to facilitate disclosure can take some time.
If patients are willing to talk about what happened to them, the situation described can be disturbing for you as well as for the patient.
Victims of human trafficking and modern slavery
Refugees and asylum seekers are at risk of exploitation, trafficking and modern slavery. This can often involve experiences of mental, physical and sexual violence.
As a healthcare provider, you may be well-placed to identify people who have been trafficked and help them to access specialist support.
Further information on common health conditions affecting people who have been trafficked and what signs to look for is available in the human trafficking section of the Migrant Health Guide. DHSC (Department of Health and Social Care) has also produced guidance and a quick two-page guide for health professionals.
The UK operates a national referral mechanism for adults and children. Adults must consent to be referred in this way. The Salvation Army can also assist with referrals.
Victims of torture and other forms of violence
Recent estimates suggest that on average 44% of asylum seekers have experienced torture, although this can vary significantly by country.
If you have patients who are refugees and asylum seekers, you should be alert to and able to identify health problems which may be physical and mental consequences of torture. However, it is important that you recognise the limits of your own competence and refer to a specialist service when appropriate.
Depending on the nature of your patient’s experiences, the most appropriate specialist service may be secondary mental health, sexual health, or support for victims of domestic or sexual abuse, or human trafficking.
The assessment and documentation of the sequelae of torture should be undertaken by experienced health professionals. The main UK centres where patients can receive specialist psychological therapy and expert assessment for medical reports to support asylum application are:
- Freedom from Torture (formerly the Medical Foundation for the Care of Victims of Torture)
- The Helen Bamber Foundation
More information on these organisations can be found in the 'useful resources'.
It is of vital importance that asylum seekers who report experiences of torture, FGM, exploitation or sexual and gender-based violence are referred on to a specialist service without delay. Proper evaluation and medical reports concerning these experiences can have a significant impact on a patient’s asylum application or appeal.
Burnout and vicarious trauma
Healthcare professionals and other staff who are exposed to disturbing patient accounts can be emotionally affected. This can include burnout as well as vicarious trauma.
Awareness and self-care along with access to education and training, regular debriefing and peer support can help you look after your own wellbeing when caring for patients who have experienced severe violence and cruelty.
If you are professionally isolated, there are migrant health forums that can connect you with a community of other UK practitioners working with vulnerable migrants.
The BMA also provides 24/7 access to our wellbeing support services, which offer peer support and professional telephone counselling, including with trauma specialists. The service is open to all UK doctors and medical students.
