It is roughly one year since the COVID-19 pandemic upended everyday life and began exacting its terrible toll on lives and communities throughout the UK.
For the majority of 2020, doctors and healthcare staff battled valiantly to check the spread of a contagious and poorly understood virus, one for which there was no standardised or proven treatment.
The sense of relief and hope that greeted the arrival of the first vaccine, approved and licensed for use in the UK in the autumn of 2020, was perhaps even greater for the exhausted ranks of the medical profession than for the rest of the country.
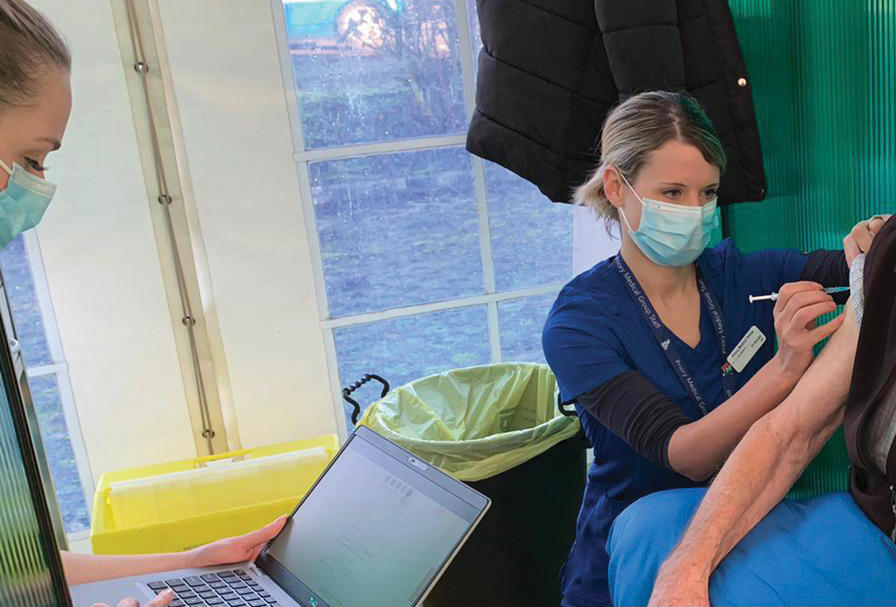
Beginning in earnest in December, the roll out of the Pfizer BioNTech and Oxford/AstraZeneca vaccines has finally provided the health service with the means of preventing infection and ultimately bringing an end to the pandemic.
You just feel that warm glow of feeling like you are contributing to moving towards an end point in this pandemicDr Brooks
With more than 3.5 million people reported to have received their first vaccine doses by 16 January, there is growing confidence among many doctors that the tide can be turned against COVID-19, provided this rate continues to grow.
‘It’s been incredibly emotional and very motivating,’ explains Watford GP Simon Hodes.
‘The patients are unbelievably grateful and the atmosphere in the clinic is almost like a carnival. A lot of these patients haven’t been out of their houses for months on end, they’re frail and elderly and have not seen their children or grandchildren for long periods of time.’
Service as usual
 HODES: 'It's more than just a transactional relationship'
HODES: 'It's more than just a transactional relationship'
Dr Hodes is a partner at the Bridgewater practice, whose premises are being used for the vaccinations, the process for which is being overseen and implemented by the Grand Union PCN (Primary Care Network) of which the practice is part.
He says his practice made a concerted effort to continue to provide normal services while conducting the vaccination programme by working overtime and bringing in volunteers.
‘We did not want to jeopardise normal services,’ he says.
‘All the problems we had seen earlier on in the pandemic of people complaining about not being able to access their GP ... in our minds to cancel any other services, routine or acute, to prioritise the programme didn’t feel right.
‘I think when you’re a GP for a long period of time, a lot of these patients become friends. It’s more than just a transactional medical relationship, you become part of patients’ lives and vice versa.’
This mutual sense of joy and relief with the arrival of a vaccine is something York GP Abbie Brooks understands too.
A partner at the city’s Park View Surgery, she and her colleagues have since 21 December been administering doses of vaccine at a central hub and through visits to care homes, an effort organised by the Nimbus PCN.
‘Outside of the hub there is sometimes frustration from relatives or patients that they have not yet been invited for vaccination, but you don’t feel any of that on the ground,’ Dr Brooks says.
‘You just feel that warm glow of feeling like you are contributing to moving towards an end point in this pandemic.’
Jab gap
 HODES: Receipt of vaccines something of a lottery
HODES: Receipt of vaccines something of a lottery
Many aspects of the response to the pandemic have been administered by the private sector, with the likes of Deloitte entrusted with managing drive-in COVID testing centres and Serco being involved in the contact-tracing programme.
By contrast, the COVID-19 vaccination programme was entrusted to general practice as part of an enhanced service agreement between NHS England and Improvement and GPs.
While the roll out has so far seen a slow but steady rate of progress in increasing the numbers of those being vaccinated against the virus, challenges and difficulties remain.
There is still contention with the Government’s decision to increase the wait time between initial and booster doses of the vaccine from three to 12 weeks, while issues around ensuring consistent supply of the vaccines to practices and hubs also remain.
Dr Hodes says ordering vaccines took place through an online portal and it was often something of a lottery as to whether you would receive the vaccines, which type they would be and when they would arrive.
The patients are unbelievably grateful and the atmosphere in the clinic is almost like a carnivalDr Hodes
‘Deliveries are extremely sporadic and unreliable,’ says Dr Hodes.
‘We went to get a delivery of the Pfizer vaccine last Wednesday [13 January], only to receive an email at 4.30pm on the Tuesday to tell us it wasn’t coming, meaning we had to frantically phone around to cancel with patients.
‘It’s not unique to our practice and has happened a lot around the country.’
Dr Hodes also expresses frustration with the decision to open mass vaccination centres, something he said has resulted in some patients receiving conflicting notifications as to where they should attend to receive the vaccine, with this confusion creating extra administrative burdens for GPs.
Added to this, and problems with supplies, are the challenges presented by storing and administering the Pfizer vaccine which has to be reconstituted before use, has a relatively short shelf-life and requires patients who receive it to be observed for 15 minutes following vaccination.
‘It’s been an incredible amount of work just organising the logistics around the Pfizer vaccine because it’s so time-pressured when it arrives at the practice,’ says Dr Hodes.
‘It’s a new process for us. Normally, the vaccines we get are just ready-made in a syringe with a needle on the end, you get them out of the fridge, pop them in someone’s arm and off they go.’
Safety first
By contrast, while supply of the vaccines has become more consistent from Dr Brooks’s point of view, providing the vaccine to so many patients while accommodating other health needs and meeting the safety requirements, remains a challenge.
‘The challenge there is just doing it as safely as possible,’ she says.
‘In the first round we would go in to do a whole home, but if there are new residents joining then you keep having to go in to “mop up” as it were which is a challenge.
‘Every time you go into a home you have to have a negative lateral flow result, take your own PPE [personal protective equipment] and consent forms.
‘While care homes are absolutely the right thing to prioritise, it is a lot of work to continue to keep those homes vaccinated.’
While care homes are the right thing to prioritise, it is a lot of work to continue to keep them vaccinatedDr Brooks
 BROOKS: 'Huge number of patients'
BROOKS: 'Huge number of patients'
She says at her practice more than 70 per cent of those aged over 80 have now been vaccinated, with one of the oldest patients being more than 100 years old.
‘It’s a huge number of patients and frailty and mobility issues mean that you have to ensure there are wheelchairs and people to assist at the [vaccination] hub. These patients have multiple co-morbidities, so observation is key,’ she says.
‘When we start to move down the age groups, I think things will start to move a bit faster.’
The Government’s Joint Committee on Vaccination and Immunisation has stated it aims to ensure every adult in the UK aged over 18 has received at least a first dose of a COVID vaccine before the end of this year.

