ICPs (integrated care providers) are population-based models of care that integrate primary, secondary, community and other health and care services under one single provider contract.
ICPs are distinct from sustainability and transformation partnerships (STPs) and integrated care systems (ICSs), both of which focus on achieving integration without contractual change.
What integrated care providers are
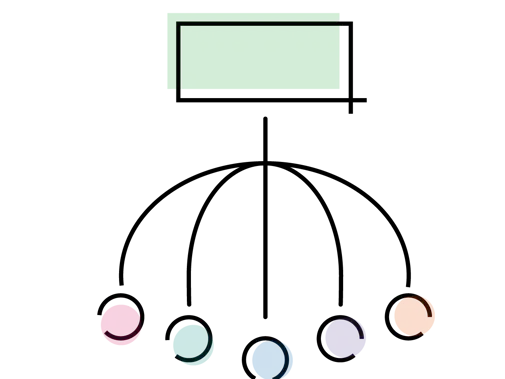
An ICP brings together a number of providers to take responsibility for the cost and quality of care for a defined population within an agreed budget.
The key feature of an ICP is that there will be a single contract with a single organisation for the majority of health and care services in the area. The ICP contract holder would be responsible for the provision of services, but may not necessarily deliver all the services itself. It could instead hold sub-contracts with other providers.

The BMA position on ICPs
We agree that there is a distinct need to better coordinate and integrate health services which will use NHS resources in a cost-efficient manner.
We do not believe that new contractual models are required to achieve this. The same outcomes can be achieved using existing frameworks. ICSs, for example, operate on the basis of allowing integration with local agreements without the need for formal contracts.
We have several concerns regarding ICPs. These include:
- the lack of clarity and accountability surrounding their development so far
- the risk of privatisation they present - current procurement law means that combining multiple services into one contract risks the potential for non-NHS providers taking over services for entire areas
- whether Government will provide the level of NHS funding and investment required for them to work
- how they will secure the future of general practice.
The impact of ICPs on GPs
GP practices will be required to sign up to the contract in order for it to operate. However, GP practices do not need to enter into this contractual agreement.
BMA concerns
ICP contracts will undermine the GMS contract and the partnership model of general practice. The GP partnership review found this provides practices with plenty of initiatives, such as autonomy and value for money.
Protections for GPs
GPs must have protections in place so that if they reject the proposed models they have a commitment that:
- their contracts, funding and services are ring fenced
- they will have the flexibility to agree the contractual arrangement with the ICP
- there will be the option for them to unlock further funding via (potentially) a separately commissioned contract to achieve this integration
The ICP contract contains requirements that salaried GPs must be offered terms no less favourable than the BMA model contract, as per GMS regulations. We expect all doctors employed under an ICP to be provided with nationally negotiated terms and conditions.
If GPs choose to operate under an ICP contract
If a GP practice chooses to operate under such a contract there are two options.
Partial model
Member practices retain their core GMS/PMS contracts but sign a separate ‘integration agreement’ to operate under the ICP provider.
Full model
The practice core contract is ‘suspended’ and replaced in their entirety by the ICP contract.
Right to return
GP practices working under the ICP contract will have a 'right to return' should they agree to suspend their GMS/PMS contract and integrate fully into an ICP.
Whilst it will be possible for a practice to return to a 'suspended' GMS or PMS contract there is no guarantee that the practice will return to an adequate level of funding.