What needs to change to improve care for patients and the working lives of doctors in the NHS?
For more than a year the BMA has sought to answer this question through the caring, supportive, collaborative project.
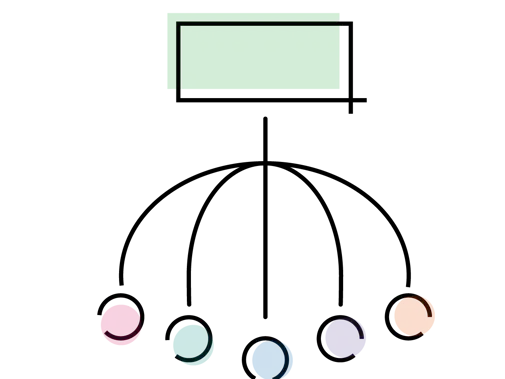
Within the three key areas of workforce, structure, and culture, we have set out our priorities specifically for government.
Our manifesto
We set out the key issues which government must work to address to deliver a truly sustainable NHS. One which is underpinned by adequate funding and terms and conditions for doctors to relieve system pressures. One which is caring, supportive and collaborative.
An environment that supports doctors’ wellbeing, promotes learning and encourages the development of systems to improve safety and quality of care. Where diversity is celebrated and there is equal opportunity and reward.
Regulation
It is vital that doctors and clinical staff are given adequate time and facilities to be able to reflect on their experiences. They must also be freed from the pressure of a regulatory system which seeks to blame, not learn.
CQC
Review the CQC with the intention of introducing reforms which will deliver a truly proportionate regulatory system.
GMC
Introduce amendments to the Medical Act to allow the GMC to streamline its fitness-to-practise processes which are inflexible, heavy handed and place great stress on doctors.
Management
Introduce a regulatory mechanism for NHS management which will ensure core skills are maintained with clear individual accountability.
Where everyone who works in the NHS feels part of a properly resourced team working in harmony and with the right mix of skills to do the job.
Pensions
Scrap the punitive tax and pension regulations which are driving senior doctors out of the workforce. Without action the staffing of services will be left in jeopardy.
Safe staffing
Introduce legislation in England to ensure system-level accountability for staffing levels, which will make sure that individual clinicians are not blamed when the system places them under unmanageable pressure.
Pay
Deliver pay increases which truly value our medical workforce and help to retain staff. Commit to introducing a mechanism to address historic underpayments to doctors.
Where doctors and all NHS staff are empowered to work together across traditional organisational divides, so that patients receive seamless care.
NHS funding
Address the funding gap by increasing spending across the UK by at least 4.1% per year to put the NHS on a sustainable longterm footing. This equates to an extra £9.5bn by 2023/24.
End wasteful competition
Deliver on the NHS’ desire to revoke legislation in England which has led to wasteful competition in the NHS and restore the NHS as the preferred provider of services.
IT
Invest in a comprehensive IT programme so the NHS has access to the right IT equipment and facilities to provide the best care for patients.
This includes basic IT infrastructure and access to high-speed broadband.
Report: doctors’ vision for change in the NHS
This report draws on the experience and expertise of BMA members.
It outlines where we believe we need to see change to ensure we safeguard patient care, make the NHS a great place to work and transform services for the better.
Doctors want to see:
- an NHS that has a culture that is not rooted in blame, but supports and encourages learning and improvement, celebrating diversity so that everyone has the opportunity to succeed
- an NHS that values its workforce as its strongest asset and supports doctors to be able to work safely, with the right mix of skills to meet the changing needs of patients
- an NHS set up to encourage collaboration across traditional divides, and where money is spent on delivering patient care.
Recommendations
Our report sets out recommendations aimed at government and NHS bodies.
Doctors have suggested, for example, that the way patient safety incidents are investigated should be radically changed to ensure that they can be seen as opportunities to improve future care rather than assigning blame.
In addition, in line with recent development in Scotland, new legislation is needed in England to create much clearer lines of accountability for safe staffing.
Investment in IT systems, that work across different parts of the NHS, is also needed to ensure that patient information can be securely shared between clinicians and with patients.
All these changes must be underpinned by sufficient resources to reverse the underfunding that has left the NHS in crisis over the last decade.
Working closely with partners across health and social care, the ideas contained in this report take us a step closer to building an NHS that is truly caring, supportive and collaborative.
Survey
Doctors tell us there is a persistent culture of fear across the NHS, where blame stifles learning, contributing to the vicious cycle of low morale and poor rates of recruitment and retention. Doctors are leaving the profession due to a feeling of being undervalued and being hit by punitive pension taxation. All of which has a knock-on impact on the patients and their care.BMA council chair, Chaand Nagpaul
In May and June 2018, doctors across the UK were invited to share their views on a range of issues affecting their working lives and focusing on three themes: culture, structure and workforce.
The report sets out the responses we received, which together provide a clear picture of the challenges and opportunities facing doctors in the NHS today.
Just under 8,000 members completed the survey.
Future vision for the NHS roundtables
In March 2019, we hosted two roundtable events with leading figures including the including the Secretary of State for Health and Social Care, Matt Hancock MP, and NHS England Chief Executive, Simon Stevens.
These roundtables enabled senior elected BMA members to lead discussions about the practical changes needed, such as:
- how quality and safety of care is compromised by the barriers between primary and secondary care
- scrapping current competition rules
- how we might develop a health service culture which supports and encourages learning and improvement, rather than one which is rooted in blame, and the role of regulation
- the inspections approach of the CQC.
Report: better culture, better care in Northern Ireland
Collated following the better culture, better care conference in Belfast, this report outlines work being undertaken across the UK on what a caring and trusting environment could look like for doctors and patients.
An individual duty of candour with criminal sanctions is being considered in Northern Ireland. This is causing considerable concern for doctors who fear it will reinforce a culture of blame and sanction rather than openness and learning.
Report: secondary care matters in Scotland
Developed by Scottish consultants as part of the project, the report sets out a principles-based approach to shaping the future of safe, sustainable secondary care in Scotland. It contributes to the debate of how to transform the planning and delivery of secondary care.