Receiving results ordered by another clinician
Traditionally a clinician who orders a test is responsible for receiving and acting upon the results once available.
This may require direct action by the clinician or a transfer of responsibility, for example a consultant writing to the patient's GP with the details of the results and any actions.
Likewise, if tests are required as a pre-requirement for a hospital referral, a GP would be responsible for making the hospital aware of the relevant results as part of the referral process.
Until an explicit code of practice is agreed, clinicians should assume that the ordering clinician is responsible for receiving and acting upon results and should not assume that others who can view the result will take action.
Allowing others involved in a patient's care, to view or at times act upon test results prior to the results being communicated by the 'ordering' clinician can offer benefits.
If a patient attends a GP practice shortly after being discharged and prior to the test results being formally communicated by the requesting consultant, 'pulling' down and viewing the relevant test results may help the GP decide how to care for the patient.
Test results can also be automatically sent or 'pushed' to GP practices. An automated feed of test results can blur the lines of clinical responsibility. Once you receive a test result you may also assume clinical responsibility to act upon it or ensure that it is actioned even if you are unsure whether any action has been taken.
A test result may reveal the need for urgent intervention. If no action was taken and a patient came to harm the viewing clinician could be held accountable even if they did not order the test.
We recommend that systems which automatically send test results to clinicians who have not ordered the test should be approached with caution.
If a patient is admitted following a visit to the emergency department, the consultant now caring for the patient may wish to view the results of test ordered by the emergency department. There needs to be clear local protocols about who is responsible for taking action.
Instructing another clinician to take action upon a result
Sometimes a patient will have left your care when test results become available. In most cases it is appropriate for the ordering clinician to review test results and forward the results with advice and comments to the treating clinician.
There may be times when you order a test but require another clinician or team to take direct action. For example, a consultant may discharge a patient when test results are pending and wish the results to be sent directly to the GP practice.
This could be enabled in system design but would only be appropriate if:
- it is clear which individual or team will be caring for the patient once the test results are available - for transfers within hospitals this may mean updating systems with the location of the patient
- there is no need for the ordering clinician to review the results prior to them being sent to another clinician
- the receiving clinician has access to the relevant clinical information to place the test results in context - for internal transfers in hospitals, patient's clinical information should be readily accessible from the test results screen
- there is a clear instruction that the receiving clinician needs to take action - you should not assume that because a clinician can view a result they know that action is required; the ordering clinician will retain responsibility until there is an instruction otherwise
- it is clear who is responsible for chasing or following up if the results do not arrive - if the receiving clinician is located in a different organisation it may not be possible to track the results down.
Electronic results and hospital teams
Electronic systems need to offer safeguards ie:
- results need to be available to all those involved in a patient's care
- clearly marked with who ordered them
- who currently has responsibility for them
- who has looked at them and who has signed them off
- users to log on as an individual but still have access to all the relevant results for checking and cross checking.
It is important for hospital teams to have a clear policy relating to the review of results and any subsequent action. The ultimate responsibility will lie with the consultant responsible for the patients' care. Any delegation must:
- be clear
- result in an appropriate audit trail
- be flexible enough to manage planned and unplanned absences of various team members including the responsible consultant.
When decisions are made before test results
There will also be situations in hospitals, where clinicians will need to make a decision prior to results being available. It is important that once the report is available, it is used to ratify the original diagnosis or treatment even if the patient has already been discharged.
If the results do not confirm the accuracy of the diagnosis then further action may need to be taken even if that is simply informing the patient and their GP of the findings.
Communication of critical results
Results relating to potentially life threatening problems should be communicated directly to clinicians caring for patients.
All organisations should ensure that clear policies for communicating critical or life threatening results have been implemented.
The results may include (but not be limited to) critically high potassium levels, grossly abnormal renal function, cancer diagnoses, grossly abnormal radiographs and in some instances cardiac biomarkers. In these instances the laboratory generating the result should telephone the responsible clinician.
Shared team inboxes
A procedure should be in place so results are actioned when they arrive in to a team inbox.
Thought should be given to:
- how results requiring immediate action should be dealt with
- who should review results during absence of a team member
- how these procedures are communicated to those who are not regular members of the team eg locums
- making someone, eg the secretary, responsible for flagging and following up unactioned reports on a regular basis.
Shared electronic records
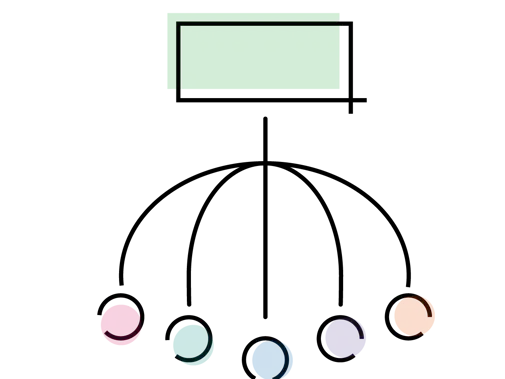
With more than one health professional having access to a shared electronic health record, there needs to be a system which can analyse the results and send alerts to the 'responsible' health professional, who may differ from the person ordering the test (eg in patients recently admitted to or discharged from hospital).RCGP - Shared Records Professional Guidance
- There must be processes in place to ensure it is clear who is responsible for acting upon a result.
- it must not be assumed that because others can see the result in the shared record they will know to take action.
- Generally the clinician who ordered the test will retain the responsibility for taking action or delegate action.
- It should be clear to others viewing the record when a result has been signed off and by whom.
Results sent electronically by patients
Some patients capture their own health information following advice from a clinician or because they want to.
Patients may bring measurements to their appointment. In the future it may become more commonplace for clinicians to receive a feed of patient taken measurements, with agreement.
What you should agree
- The responsibilities on each side, eg the timescales for follow up.
- What patients should do if they take an abnormal reading, eg going to the emergency department if they take an abnormal reading in the middle of the night.
- That you assume responsibility for taking action on the measurements when clinically necessary.
Processes
- It would be useful if electronic systems could be set up to filter measurements so alerts are generated for abnormal readings.
- Once receiving an alert the clinician would be responsible for considering the reading and deciding the action to be taken.
This would include if you decided to access results out of hours remotely from home and viewed a result, which required urgent attention. - Considerations need to be made for shared records; if there are multiple clinicians accessing a shared record, who is responsible for taking action?
- The clinician who asked the patient to submit measurements, or who had an agreement with the patient, would be responsible for acting upon the information. That is, unless they turned up in another setting, eg out-of-hours.