General practice in Northern Ireland is in crisis. Over 17 practices have handed their contracts back since January 2023 and those that remain are stretched. GP training is undersubscribed, meaning fewer GPs of the future. We are seeing an unsafe service in every area. In Northern Ireland we have published our plan to save general practice, which details what we think needs to change to stabilise general practice.
One of the points of this plan was to define what ‘working safely’ should mean in the current context. The purpose of this guidance is therefore to support GPs and their practices in difficult circumstances to safely manage their workload to a safe level. It can also be used as a guide by all practices to assess whether their level of service provision and patient access is consistent with our recommendations. It is hoped that this guidance will help practices to establish a reasonable and safe workload – to protect GPs, their staff, and patients – and ultimately help maintain GP services in the long term.
This advice is specifically for GP practices operating under the national General Medical Services (GMS) contract. Practices operating under an Alternative Provider Medical Services (APMS) contract should contact their local medical committee (LMC) for advice.
Defining safe working levels
Until there is better support and funding to reverse the sustainability crisis, GP practices must be prepared for increasingly difficult circumstances and further workload challenges. Many practices will need to protect themselves and their patients from the unsafe consequences of excessive workload.
The GP practice workload crisis is often so serious that we recommend practices take urgent action to preserve patient care and their own wellbeing. Practices will need to decide how to prioritise care and day-to-day activity accordingly. These actions will inevitably result in some patients waiting longer, or issues that do not need to be dealt with in general practice being directed elsewhere.
The Department of Health (NI) and the Strategic Planning and Performance Group (SPPG) are ultimately responsible for the provision of primary medical services to patients. While SPPG contracts with GP practices to deliver this responsibly, GP practices are not a safeguard for all NHS services or providers of last resort. We cannot be expected to operate beyond the terms of our contract or undertake a workload that is unsafe.
1. GP practices can limit their workload and direct patients to other NHS services
GP practices can limit their workload, consistent with the advice that follows, to protect themselves, their staff, and patients. It is acceptable for GP practices, where they have reached their safe working limit, to direct patients to other NHS services. If other NHS services are unable to see patients, that is not the responsibility of the GP practice. Practices can direct emergency and urgent problems to other NHS services including Urgent Care Centres, Phone First, GP out-of-hours, Accident and Emergency, and the Northern Ireland Ambulance service.
Practices may wish to consider, when they have reached their safe maximum activity for a day, to respond to further patient phone calls with the following message. It is hoped that practices will very rarely need to do this and we advise any practice doing so to inform SPPG.
Message to patients where safe practice capacity has been exhausted:
"The practice is currently experiencing unmanageable demand for urgent care. Taking account of our patients’ and practice team’s safety and the availability of other options for patient care we are not able to see any more patients today. We are sorry for this inconvenience, which is beyond our control. If you have an urgent medical problem that you believe cannot wait, then you should seek help from other NHS agencies including Phone First or through accident and emergency."
2. A safe level of working for all GPs is 25 patient contacts per day
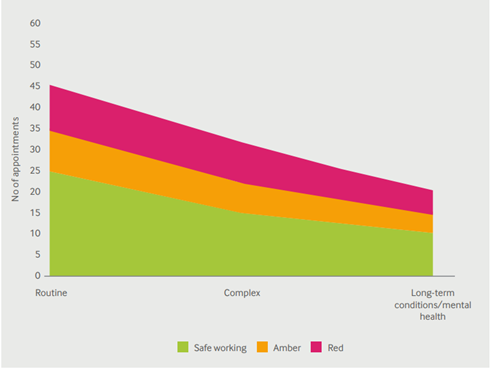
Safe working in general practice (BMA 2018) The number of safe patient contacts reduces as complexity of the contact increases. Our advice on a safe number of appointments was published in 2018. We expect that 25 patient contacts per day includes a mix of face-to-face and remote contacts. We believe the complexity of patient contacts is generally increasing and resulting in more non-patient-facing clinical tasks.
3. Safe working levels should apply to duty doctors
Many practices in Northern Ireland operate with a duty doctor that picks up urgent and unscheduled care. This can be efficient – allowing other GPs to focus on planned care delivery – but also risks uncontrolled and excessive workload which is not consistent with safe working. As detailed above, it is important to have a policy for diverting urgent care needs where they cannot be met safely by the practice.
We are aware this could be difficult to implement for all practices but innovative approaches have allowed practices across Northern Ireland to protect all GPs from unsafe workload demands. Practices need to be aware that there is no requirement under the GMS contract for GP practices to have a duty doctor and we are increasingly concerned that duty doctors are working beyond the levels recommended in this guidance.
Successfully applying this guidance means that duty doctors cannot and should not act as a sponge to soak up demand from patients who are finding access to the practice slower than desired. Where practices choose to operate a duty doctor system, they should consider having clear policies for the type of contacts that is appropriate to be passed to a duty doctor. Practices may also wish to consider indicating to patients that a message about their call will be passed to the duty doctor to consider, but that the duty doctor will only call back where it is clinically urgent and there is sufficient capacity in the practice to allow them to do so, rather than creating an automatic expectation of a duty doctor consultation.
4. GP practices can book 15-minute appointments for all patients
We strongly recommend practices take immediate measures to move to 15-minute appointments. Most practices still provide care at 10-minute intervals. This includes patient note-keeping and other non-patient facing clinical tasks between seeing patients. Without increasing the total time spent on consulting in a day, GPs can preserve quality of care by moving to 15-minute appointments.
We recommend that no more than three hours per session is spent in consultation with patients to allow adequate time for clinical administrative tasks. Within these limits, adequate rest breaks must be taken. Extending sessions beyond this time risks harm to patient and clinician. Increasing appointment lengths to 15 minutes would mean a reduction in the absolute number of appointments per session to safe levels for clinicians and patients.
Methods of controlling workload
In addition to the measures above, there are several options for practices under the GMS contract to protect themselves from unmanageable workloads. While no single option is likely to be a complete solution, it may be possible through a variety of measures to reduce the workload of a practice to a level that is safe and manageable in the longer term.
1. Inform SPPG and consider local escalation processes
Let SPPG know that workload at your practice is regularly reaching an unmanageable/unsafe level which is impacting on your ability to provide safe care for your patients. Formally write to SPPG informing them that your practice workload is unmanageable and that you are seeking the SPPG’s support to resolve the problem. SPPG are ultimately responsible for primary care and have a responsibility to support practices.
When writing to SPPG, communicate the reasons why the practice workload is unmanageable. Reasons may include (but are not limited to):
- the patient list being too high
- unfilled vacancies/inability to recruit GPs or other practice staff –
- inadequate or unreliable SPPG services to patients – inadequate space to accommodate the practice responsibilities
- insufficient financial resource, etc.
- the impact of long waiting times for hospital appointments
- inappropriate/unfunded transfer of work from secondary care
- increasing burden of non-clinical tasks
- ES returns, redaction of records etc
You will also want to highlight any practical help SPPG could provide to improve the situation, such as referral to the Practice Improvement and Crisis Response Team (PICRT). Practices will want to consider SPPG’s reply and any suggestions that might improve your workload. If SPPG does not respond promptly or you do not consider their response helpful, you should consider implementing other aspects of this advice as you deem necessary.
You should also inform your LMC of your practice workload difficulties. LMCs are helpful in highlighting any local support or systems in place that could help your practice. In Northern Ireland local escalation processes are in place that allow practices to reduce their services to patients if faced with serious capacity challenges.
2. Consider reviewing practice arrangements for patient access
GP contractors are required to carry out their obligations under the contract with reasonable skill and care and to provide for their patients’ reasonable needs. Practices must exercise their professional judgement in allocating their resources in accordance with their usual ways of working. This applies to the processes the practice puts in place to allow patients to access the services they provide. Practices should regularly review their access arrangements to ensure the best for patients within their practice capacity.
GP practice capacity is finite. If demand exceeds capacity, then practices may prioritise care for those patients with the greatest need. Unfortunately, not every patient can be seen when they wish. It is reasonable for GP practices with unmanageable workloads to limit either the number of appointments they have or to increase appointment length.
If safe working capacity is reached, patients could be placed on a practice waiting list. This would be a significant new way of working for practices and would have considerable administrative workload and possibly clinical governance aspects that the practice would need to carefully consider.
General practices can adopt the approach of secondary care which has waiting lists based on clinical need. This approach will result in some patients waiting longer for an appointment with their GP but will allow GPs to focus their resources on those with the greatest need. A patient’s clinical condition may well change while on the waiting list and a practice may consider reviewing the urgency at this point. Alternatively, they may consider directing the patient to another NHS service. Practices should advise patients placed on a waiting list to call the practice again if their condition deteriorates.
3. Pushing back on inappropriate workload
We have provided template letters to support GP practices in pushing back on inappropriate work from secondary care, prescribers, and other health services. Practices may use these templates where they consider that requested work is inappropriate. LMCs and the BMA can help practices determine if work they are being asked to do is inappropriate.
4. Managing patient complaints
Patient complaints can be a significant source of anxiety and stress for GPs, particularly when they occur despite GPs going above and beyond to care for their patients in the face of workload challenges. Practices may worry that implementing safe working limits could lead to their practice receiving more complaints from patients who are frustrated at the level of access to appointments that the practice is able to provide.
It is important, however, to recognise that the amount of capacity that practices have available and the number of appointments they can safely offer is ultimately driven by the government’s investment and workforce planning decisions and the level to which it wishes to prioritise general practice. While practices have flexibility in how they deliver their services, they do not control the overall funding envelope that can be used to deliver GP services, nor do they have responsibility for ensuring sufficient new GPs are trained and existing GPs are incentivised to remain in practice.
Complaints about access to appointments are often complaints indirectly about government policy. While practices must treat all complaints seriously, they can and should highlight this fact to patients and may wish to suggest patients contact their MLA or the Department of Health to make clear that general practice needs greater resourcing to be able to provide more appointments.
Practices should also recognise that the risk of more serious complaints relating to standards of patient care falling short of what a patient expects are more likely to occur when clinicians are working beyond capacity and at increased risk of making mistakes. Implementing safe limits on workload can help reduce the chances of such mistakes occurring and serious complaints being subsequently received.
5. Consider formal practice list closure
Practices can notify SPPG that they wish to close their patient list to achieve a more manageable and safer workload. Practices wishing to close their list will need to apply to SPPG. Following receipt of such a request, SPPG will have 28 days to enter discussions with the practice to resolve the practice’s concerns. This will include discussing what support SPPG can give to enable the practice to keep its list open.
Practices should consider our advice above on safe working to determine a reasonable list size that would trigger the reopening of the list. SPPG can reject applications by practices to close their list following consideration by an assessment panel. This decision can be challenged via an appeal. Patients can continue to be allocated to practices with a closed list by the BSO in an area where most practices have a closed list.
6. Consider reducing your practice area
Practices can apply to SPPG to reduce their practice area. This can help control the size of the practice list and limit travel for home visits. SPPG’s decision process for such requests is similar to the process for requesting formal list closure. Practices can apply to change their boundary once per year and should apply at the beginning of each financial year. SPPG will review the request and should inform the practice of the outcome of the decision and reasons for refusal if the application is declined.
7. Consider reducing provision of voluntary services
Practices are not obligated to provide additional or enhanced services (local, national, or directed). Practices that wish to cease additional services can opt out under the contract or advise SPPG if they wish to cease enhanced services. This will impact practice funding. Practices should consider whether it is protective or cost effective to continue providing additional or enhanced services.
Practices may also wish to review the services they provide for chronic disease management which have never been funded contractually for repatriation back to hospital; for example, spirometry provision. We have produced a list of services that are not considered to be part of GMS and would normally attract funding in an enhanced service.

