At your GP practice, you need to understand the requirements to register and provide services to patients residing in institutions or care homes where the types of services expected may not fall under your contractual obligations.
When GPs provide services to patients residing in institutions and care homes, there is often confusion over who is clinically responsible for their care. This may present a risk to patient safety. You must not be forced to accept clinical responsibility for aspects of the care of patients in secondary care institutions, nor for those in any setting where the clinical needs of the patient fall outside the normal skills and contractual requirements of GPs.
This guidance outlines the responsibilities of practices in deciding whether they need to register such patients and what services they are required to provide if so.
Your practice's obligations to register patients
There are limited grounds by which a practice may refuse to register a patient who is a temporary or permanent resident within the practice boundary, under Part 2 paragraph 21 of Schedule 3 of the GMS regulations (2015).
There are some circumstances in which “reasonable grounds” may apply. You should assess these on a case-by-case basis.
Practices should only register patients where it is believed the individual wishes to register. Institutions should not register patients without the individual’s consent.
Intermediate care
There is a trend to discharge relatively high-dependency patients from hospitals to other institutions, with GPs increasingly being asked to provide care which is likely to be beyond that which most GPs are trained or contracted to provide. Care for patients in intermediate care can also present problems caused by a lack of clarity about the professional responsibility of GPs.
There is national funding for virtual wards and many areas have Local Incentive Schemes or Enhanced Services for provision of intermediate care. It is therefore the responsibility of commissioners to employ either virtual ward funding or a locally commissioned arrangement for provision of intermediate care.
Registration of hospital inpatients
NHSEI’s Policy and Guidance Manual 4.11.3-4 states that “there are no legal grounds for refusing to register a patient because they are an inpatient in a hospital. Practices are not however expected to provide anything other than essential and additional services in these circumstances. If the resident requires any other services these must be arranged by the hospital or the commissioner.”
GPC England’s advice is therefore that decisions need to be taken on a case-by-case basis. Your decision should take into consideration the needs of the patient, the services provided by the institution, and any other commissioned services that may be available to the patient.
If a hospital is providing a full range of medical services e.g. acute care and is not a single speciality (e.g. a psychiatric hospital), then it is very likely the practice will have “reasonable grounds” to refuse registration. If adequate primary medical services are provided by the institution (as commissioned by the Commissioner) or if alternative commissioned arrangements are available to the patient, then it may not be necessary for a practice to register a patient who is resident in that institution. Decisions needs to be taken on a case-by-case basis.
Where it is known to the practice (remembering that the assessment and decision rests with the GP) that adequate primary medical services are not provided, current legal advice suggests there are unlikely to be “reasonable grounds” for refusing to register such patients.
Where there is need for a practice to provide primary medical services to people resident in a facility, there is a template memorandum of understanding available. BMA would also expect commissioners to agree extra support and funding to enable practices to provide services to this difficult-to-reach population.
Provision of services
Regulation 17 (5) (b) of GMS Regulations provides contractors with discretion to decide the scope of the treatment or investigations that are necessary or appropriate. This discretion must be exercised reasonably.
Decisions need to be taken on a case-by-case basis. The fact that certain services may be provided within the institution is a factor in deciding the extent of any supplemental services which it is necessary or appropriate for the GP to provide.
The view of GPC England is that GPs are entitled to refuse to provide care of a kind which the patient already receives or can receive from the institution where they reside. You can also refuse care that would be beyond the scope of normal primary medical services as defined by the GMS contract.
Prisons and other detention centres
Care of people in prisons and detention centres is a specialist service and is commissioned separately from general practice. Practices are not expected to register people who are detained in prisons or other detention centres.
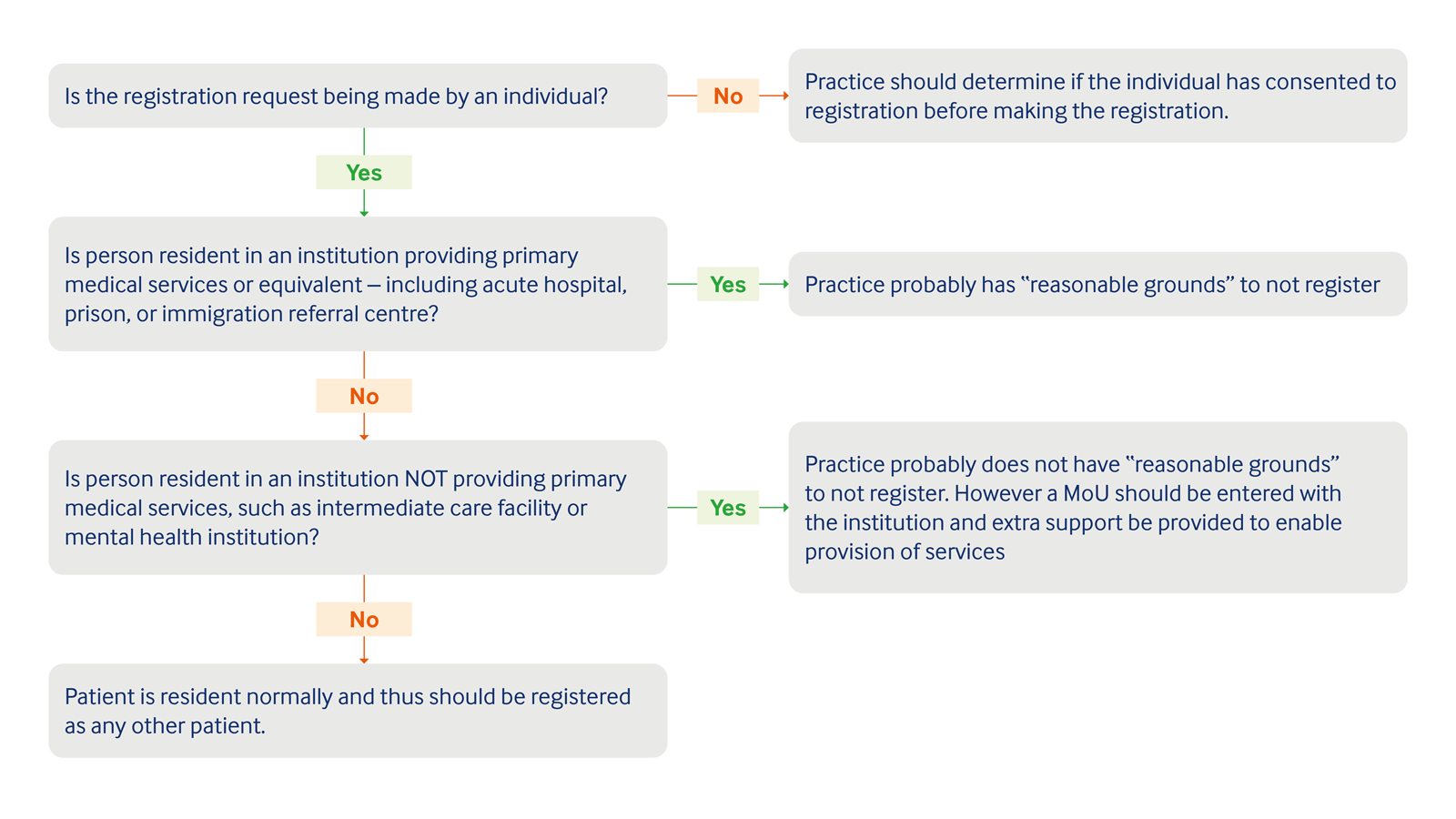
A flow chart demonstrating the decision making process when registering a patient at a GP practice.
Is the registration request being made by an individual?
- No: Practice should determine if the individual has consented to registration before making the registration
- Yes: Next question
Is person resident in an institution providing primary medical services or equivalent - including acute hospital, prison, or immigration referral centre?
- Yes: Practice probably has 'reasonable grounds' not to register
- No: Next question
Is person resident in an institution NOT providing primary medical services, such as intermediate care facility or mental health institution?
- Yes: Practice probably does not have 'reasonable grounds' to not register. However a MoU should be entered with the institution and extra support be provided to enable provision of services.
- No: Patient is a resident normally and thus should be registered as any other patient.
Obligation to carry out a visit
If you are requested to carry out a visit to an institution to provide services to a registered patient, a clinical decision should be taken on a case-by-case basis in the same way as any other registered patient would be assessed for a home visit.
Under the GMS Regulations, where in the reasonable opinion of the contractor attendance outside of practice premises is required due to the medical condition of the patient, then primary care services must be provided in the most appropriate place.
This means a request to visit a patient in an institution will not be appropriate unless the medical condition of the patient requires it. The fact a patient was detained under the Mental Health Act, lack of staff, or lack of transport would not be factors to consider if such a request was made. The memorandum of understanding allows for a “description of when a visit may be required and for what reasons in a manner determined by the practice”.
Provision of primary medical services
Even where GPs are required to take responsibility for residents or patients, there is no requirement to provide any services beyond those set out in the GP’s primary care contract. You should decline to work outside your normal clinical remit as a GP.
GPs are reminded that the definition of essential services in the GMS/PMS regulations refers to services being provided in a manner that is determined by the practice and are “necessary and appropriate”. If you are working outside of your expertise and training you put patients at risk as well as your own registration.
You need to be aware that some services simply do not fall within the normal competencies of the average GP. They should be provided only by a doctor with the appropriate specialist skills and training.
GPs who are being pressured into providing care in hospitals or are unclear as to whether an institution is a secondary care establishment and are unclear in respect of their responsibilities for both patient registration and the provision of care, should contact their LMC and their medical defence body for advice.
You should also raise concerns with the CQC (in England) over the care in any institution should you feel that safe and appropriate medical arrangements are not being adequately commissioned or provided and are putting patients at risk.
Private arrangements
Practices may also enter into private arrangements to provide administrative services to institutions, for example regular ward rounds, completion of institution medical records and drug charts, providing advice to the institution management etc. but must not charge for any services which would constitute the provision of treatment to individual registered patients.

