‘At times I felt like a sacrificial lamb. I was the young doctor in the team, we didn’t have enough masks and it was often just me there, fighting fires, which was pretty horrible.’
Mark Coulson recalls his ‘traumatic’ experience during the first wave of COVID working as a senior house officer at a London emergency department before he moved to Brisbane, Australia, in October 2020. The experience was the final straw which pushed him, as many others have done, to depart the NHS pressure cooker.
‘In the UK, it feels like you are there for damage control, maybe finding a diagnosis and treating the early stages of a disease before quickly trying to shove it out of your department because you’ve got huge lines of other sick people waiting,’ he says.
 COULSON: ‘It’s nice to feel I’m being recognised for the work’
COULSON: ‘It’s nice to feel I’m being recognised for the work’
‘You often don’t know how long patients are going to be in [an emergency department] because there are no inpatient beds, it could be 24 to 48 hours. You don’t know whether to hold or start medications.’
By contrast: ‘In Australia, the emergency department is for emergency medicine, so if patients are not sick enough to need life and limb or organ saving care it’s not necessarily our priority.
‘We have the luxury of time and resources to take that decision. I can really get the ball rolling, start the right treatments and the inpatient team carry on what I started. It’s not “they’re stable, now it’s your problem”, which is often the UK approach. I’ve got a defined role.’
Satveer Singh, who also works in emergency medicine in Brisbane, having moved in November 2020, feels the pressure and responsibility doctors face is better respected in Australia than the UK. Staffing levels are more manageable than his experiences in Liverpool and Sunderland, he says.
‘I got our emergency department rota two or three weeks prior to arriving in Australia and remember thinking “this can’t be right”. I was only down to work 40 hours a week. Your working hours are better protected here. When your shift ends, it’s mandated that you can’t be back in for 10 hours; if you are, you get paid quite a hefty sum for it.
 SINGH: ‘Your working hours are better protected here’
SINGH: ‘Your working hours are better protected here’
‘We still have on-call shifts, but they’re rostered. If you do get called in, you get paid on-call fees, and they make sure you have a 10-hour break before your next shift. There wasn’t an emergency department back home where you have someone on call just for emergencies. Everyone just picks up the flak.’
It’s a similar story for Zoe Clifford, who moved to Christchurch, New Zealand, in August 2018 having completed her foundation years in Bristol and Swindon.
‘I left before I burnt out, but I came close,’ she says. ‘My first job was horrendously unsupported, every day I wondered what I was doing with my life. We had half the staff we should’ve had. For the first six weeks I was in fight-or-flight mode. Looking back, it was unsafe. Often, the most senior person patients were seeing was someone who had been a doctor for about 20 minutes.
‘When I was on general surgery, there was one registrar and one foundation year doctor who would see every single one of the roughly 120 patients on the weekend. Here, registrars come in to look at five to 15 patients on general-surgery weekends.’
I left before I burnt out, but I came close. My first job was horrendously unsupportedDr Clifford
Dr Clifford explains how New Zealand employs ‘relievers’ – locum doctors whose role is to fill rota gaps if a hospital is short-staffed owing to illness or unforeseen circumstances.
‘If someone is off sick it’s not just “let’s grin and bear it”, like in the UK, it’s “is there a reliever around?”. And if there is no reliever, and I’m cross-covering, I get paid a lump sum because I’m doing more than one job. If I was to say the situation is unsafe, the consultants and the managers would say “what can we do?”.
‘I had one instance where I was covering four people’s jobs, so they cancelled clinic. The worst case is doing one and a half jobs, which I can handle. Whereas people get thrown under the bus in the UK.’
Professional respect
Dr Clifford notes how taking lieu days in return for working public holidays is protected in New Zealand – as long as a request is made two weeks in advance, it must be approved.
‘It’s way more powerful than an annual leave day, so you can use it if you need to sit an exam or go to something important such as a wedding,’ she says.
‘I didn’t clock that the pay was going to be much different until I’d already got the job, then I realised it’s substantially higher,’ says Dr Coulson.
‘It’s not really about the pay. I’ve never been particularly motivated by money, and can’t imagine many doctors are, especially those trained in the NHS. But it is nice to feel like I’m being recognised for the work. With higher pay comes a level of professional respect. You’re not having to pick up night locum shifts for extra cash, because you don’t need to, so you’ve got more time off, or for professional development.’
‘Exodus’
Dr Clifford says that, including on-call payments, her salary can be ‘two and a half to three times what I was earning in the UK’.
‘But it’s not about that,’ she says. ‘They treat you like a human, understand your job is hard and want to help you.'
Many doctors are making or considering such moves. In the GMC’s 2022 Workforce Report, 24 per cent of those who voluntarily relinquished their licences to practise between May 2021 and May 2022 did so to practise abroad, second only to retirement at 25 per cent.
Australia was the most popular destination for doctors moving to practise abroad (19 per cent, or 939 doctors) followed by Ireland (8 per cent, 379), New Zealand (7 per cent, 345), and India (5 per cent, 235).
A BMA survey published in December 2022 drew a similar conclusion. Forty per cent of the 4,553 respondents said they would leave the NHS ‘as soon as I can find another job’, citing pay erosion and working conditions as the main factors.
A third (33 per cent) said they plan to work in another country in the next 12 months, with 42 per cent of those preferring Australia, 20 per cent New Zealand, 9 per cent the Middle East and 9 per cent Canada.
Vivek Trivedi, co-chair of the BMA junior doctors committee, warns the ‘exodus’ will continue if the Government fails to negotiate a fair pay deal for junior doctors.
Access to training places, in the UK and overseas, is a big factor.
Dr Clifford’s hospital is funding her master’s, which earns her points towards her application for her cardiothoracic surgery training programme. She has also had courses, exams and conferences paid for, including accommodation and food.
 TRIVEDI: Exodus will continue if the Government fails to negotiate a fair pay deal
TRIVEDI: Exodus will continue if the Government fails to negotiate a fair pay deal
‘That’s so invaluable,’ she says. ‘Every exam is about $5,000 [£2,500]. In the UK, doctors pay exams as well as GMC registration out of their own pocket.’
Specialty training tends to be shorter in Australia, says Dr Coulson, although he notes programmes are ‘maybe harder to get on to’.
‘If you get on a programme, you’ve got maybe five years – as opposed to seven in the UK – but you’re not really doing service provision. If you did acute medicine, or surgery, in the UK, you’d end up doing three years of rotations you aren’t necessarily interested in. It’s more focused here; you choose a specialty and train in it. If you really gun through all your exams, and pass everything, you could be a consultant five years from starting training.’
Dr Coulson says working overseas was ‘always the plan’ for him, but he’ll likely stay longer than initially intended.
He adds: ‘A significant amount of people are reaching out to me on the practical steps. It seems that even people halfway through their UK training, or who were always really set on training in the UK, are now considering the move.’
Staying on
Dr Singh made the move after speaking to friends who already had. ‘It was always an option, but wasn’t really on my agenda until COVID,’ he says. ‘COVID increased pressure on us as a profession. I didn’t think I wanted to move to the other side of the world, then I saw how the balance was better. My plan was for it to be a short stay, maybe six months’ work, six months’ travel – but I’ve stayed.’
He believes many UK-trained doctors in Australia are monitoring the situation in the NHS and would consider returning if industrial action led to better pay and conditions for junior doctors.
But if that doesn’t happen, he warns many will get settled, either starting families or enrolling on training programmes. He recently started specialty training in emergency medicine, which he says means he will work in Australia for ‘at least six years’, until he reaches consultant level.
Dr Clifford has a similar issue in surgery.
 CLIFFORD: ‘I only came for a couple of years but ended up staying’
CLIFFORD: ‘I only came for a couple of years but ended up staying’
‘In the UK, if you’ve had more than 18 months’ surgical training anywhere else you can’t apply for core surgical training.’
She estimates ‘at least 20 per cent stay because it’s a nicer job’ but says ‘quite a lot of UK doctors do go home’ as well, because ‘family ties are a consideration’.
For her part: ‘I only came for a couple of years but ended up staying. If I hadn’t come here I probably would’ve been happy with my lot in the NHS. Now I’ve seen the other side it’s really difficult to go back. My mum suggested I’d abandoned the NHS, but the way it feels is that the UK Government has abandoned me by making life in the NHS inhumane.
‘I appreciate the NHS and what it did for me, no end. I just don’t want to work there right now. I would absolutely consider it if it wasn’t so horrendous, I wouldn’t even expect it to be as good as it is here. And that’s not too much to ask.’
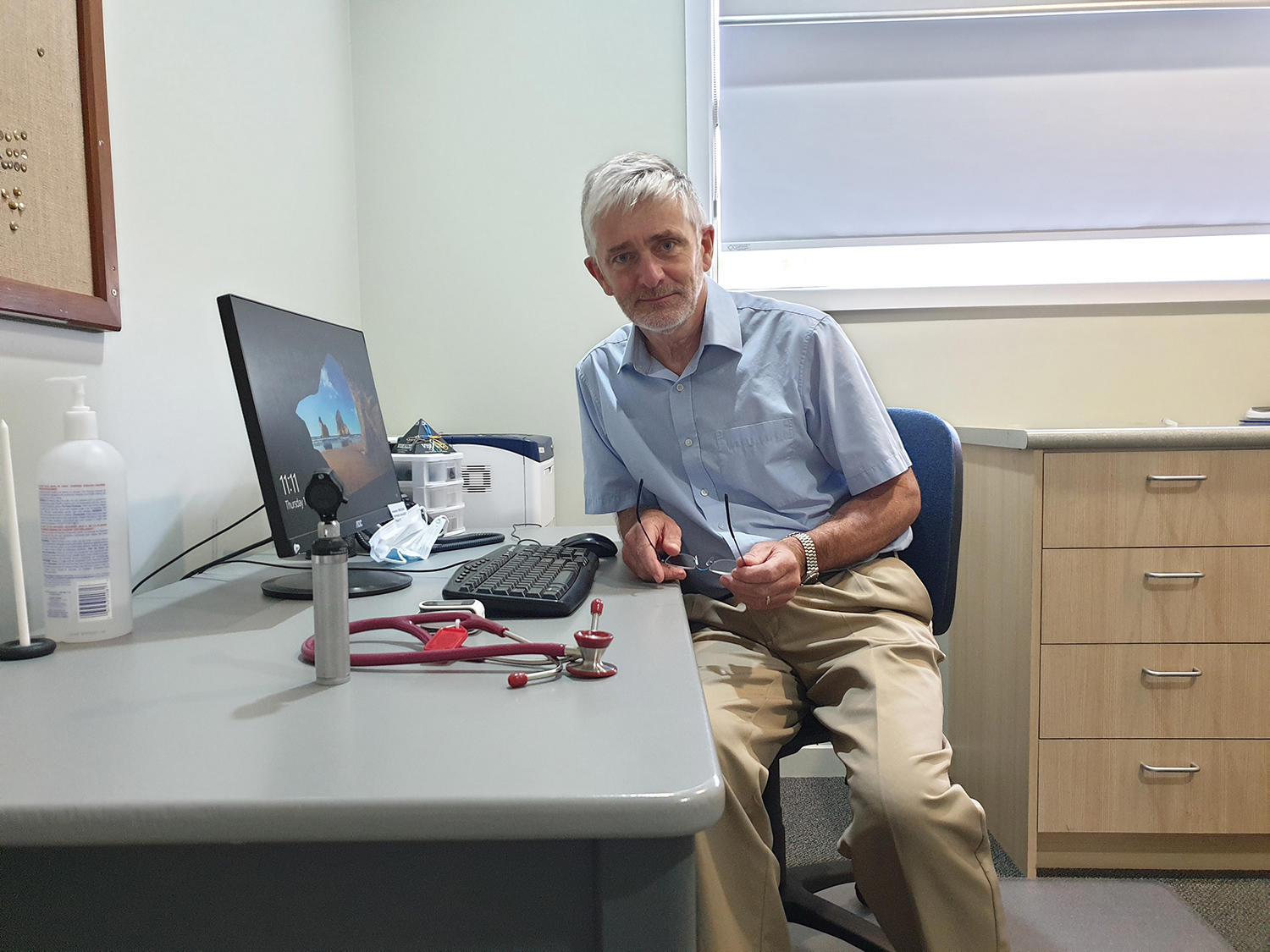 Dr Fitzpatrick
Dr Fitzpatrick
GPs follow suit
It’s not just junior doctors leaving the UK for pastures new.
The breaking point for GP Colin Fitzpatrick was flying back early from his daughter’s graduation in Exeter to cover for a locum that didn’t show up for a shift at his practice in Northern Ireland.
He is currently working in Blenheim, New Zealand, and while he plans to return to Northern Ireland he is ‘loving’ his job again after years of mounting pressure.
‘I see 20 patients a day maximum,’ he says. ‘Most days I see less. I have guaranteed lunch breaks and guaranteed time to deal with my administration.’
It’s a far cry from his experiences on the outskirts of Belfast, where three GPs – he and his wife Debbie as partners, and one salaried GP – were looking after 3,000 patients until they wound the practice up in late 2019, just before COVID.
The Fitzpatricks volunteered and ran a COVID treatment unit, with Debbie staying on as Colin took a six-month job in Queensland, Australia, where the pay was ‘shockingly high’ compared to the UK. On his return, he took roles in other parts of the UK, as a locum in the Hebrides and a medical director in Wales.
He tells The Doctor his current move is ‘basically a working holiday’: ‘We have our NHS pensions, so don't desperately need the money. It’s a life experience. I've got the mountains just over there, I'm by the sea, it’s very pleasant.’
Contrast that with his final few tears as a GP partner: ‘The workload kept increasing, secondary care were increasingly passing stuff back, probably not unreasonably, but there was no resource passing with it. Money wasn't going up and there was increasing difficulty in recruiting, especially medical staff. You just couldn't get doctors.’
‘The day we left the building there was a huge feeling of relief,’ Dr Fitzpatrick recalls. ‘It's like a weight off your shoulders. Since then, there has been some sadness. We had known some patients for decades. You really miss them and we thought we'd let them down. But on the other hand, you have to look after yourself. We meet patients in the street and they ask why, which is hard, but at the end of the day we did the right thing for us.
‘People continue because it's what they've been doing forever, and that window doesn't open for them, but we're increasingly seeing people, window or no window, just saying “I can't keep going”. I heard of a practice with six or eight partners not far from us hand their contract back. They just said enough is enough, they want a reasonable work-life balance. And I've heard several stories along those lines.’

